calsfoundation@cals.org
Vaccination
Vaccination artificially increases immunity to disease and contributes to the development of herd immunity, which is achieved when a sufficiently large percentage of immunized individuals reduces the likelihood of disease transmission. Beginning in the nineteenth century, vaccination became an essential part of American public health policy. In Arkansas, starting with the introduction of school smallpox vaccination requirements in the late nineteenth century, vaccination became a vital feature of modern public health policy.
The smallpox vaccine, discovered by British physician Edward Jenner in 1796, was the world’s first vaccine and remained the only human vaccine available until 1885. Following the introduction of the smallpox vaccine into the United States in 1800, Massachusetts became the first state to mandate smallpox vaccinations, requiring them for the general public in 1809 and for schoolchildren in 1855.
Compulsory vaccination drew both the support and the opposition of many and was subject to legal challenges. Resistance to state coercion, religious beliefs (such as those of Christian Scientists), or disbelief in the safety and efficacy of vaccines usually motivated opponents of vaccination. In Jacobson v. Massachusetts (1905) and Zucht v. King (1922), the U.S. Supreme Court upheld the constitutionality of enforcing mandatory smallpox vaccination and of excluding unvaccinated children from public school.
In 1874, Elias R. Duval, president of the Arkansas State Medical Association, proposed the passage of “a law for compulsory vaccination” in Arkansas. He did not explain whether the proposed law was to be applied to all people or exclusively to schoolchildren, and his proposal did not result in legislative action. Duval continued to praise vaccination. In 1882, while serving as chairman of the medical practice committee of the Arkansas Medical Society (AMS), he insisted that “no greater boon was ever conferred upon mankind than Jenner’s unique discovery.” On the other hand, W. H. Abington, an early-twentieth-century physician and politician from White County, claimed that the smallpox vaccine was ineffective.
In the late nineteenth and early twentieth centuries, some schools in Arkansas implemented vaccination requirements. Sometime between 1898 and 1907, the Little Rock (Pulaski County) school board began requiring, as a condition of school admittance, that students “present the certificate of a reputable physician” certifying either that they had been vaccinated against—or possessed immunity to—smallpox. In Auten v. School Board of Little Rock (1907), the Arkansas Supreme Court upheld the Pulaski County Circuit Court’s refusal to issue an order that would have compelled the city school board to allow a child who refused to present the required vaccination certificate to enter school. Citing Jacobson, the state Supreme Court opined that Little Rock’s vaccination regulation was “not unreasonable where smallpox was prevalent in the city [and] the school board [acted] under the orders of the [city] board of health and [physicians’] advice.”
In 1914, Dr. Frank B. Young of Little Rock utilized vaccination in his response to a smallpox epidemic in Elm Springs (Washington County). Young later reported that “between 800 and 1,000 people” were vaccinated during the epidemic and that “no unvaccinated person over 20 years of age [except one] recovered.”
In 1917, amid heightened concerns about the spread of smallpox during troop mobilization for World War I, the Arkansas State Board of Health instituted a school vaccination rule. The rule required teachers, students, and employees to certify either their receipt of the smallpox vaccine or their immunity to the disease before entering public or private schools. In State v. Martin and Lipe (1918) and Seubold v. Fort Smith Special School District (1951), the Arkansas Supreme Court upheld the school vaccination rule.
In the 1920s and 1930s, more vaccines—including those for diphtheria, typhoid, cholera, pertussis (whooping cough), and tetanus—became available. In 1948, the DPT vaccine (combined diphtheria, pertussis, tetanus) became available. During the Floods of 1927 and 1937, Red Cross nurses provided typhoid and cholera vaccinations to Arkansas’s flood victims. During the Great Depression, Arkansas’s public health nurses often provided vaccinations. By the early 1930s, however, many AMS members viewed the state health department’s practices of providing free vaccinations and other services as a serious threat to physicians’ fee-for-service system. After being appointed state health director in 1933, Dr. W. B. Grayson promised to end the free vaccinations and other health department practices that AMS members found objectionable.
Beginning in the mid-1950s, the newly available Salk and Sabin polio vaccines, offered through mass immunization clinics, provided protection for many Arkansas children. By 1960, the state health department provided yellow fever vaccinations at the department’s Little Rock offices and supplied the county health departments and physicians with smallpox, diphtheria, tetanus, and typhoid vaccines.
In Cude v. State (1964) and Wright v. DeWitt School District (1965), the Arkansas Supreme Court addressed two religion-based legal challenges to Arkansas’s school smallpox vaccination requirement. In Cude, the court held that the right to religious liberty did not mean that persons could “engage in religious practices inconsistent with the peace, safety and health of the inhabitants of the state.” In Wright, the court ruled that the vaccination mandate did not “violate the constitutional rights of anyone on religious grounds or otherwise.”
During the 1960s, the measles, mumps, and rubella vaccines arrived, and the combined MMR vaccine became available in 1971. Nationally, routine smallpox vaccination ended in 1972. Passed in 1967, Arkansas’s new school vaccination law mandated that children, as a condition of admission into the state’s public or private schools, medically certify that they had been vaccinated against polio, diphtheria, tetanus, pertussis, measles, and (after 1973) rubella. The law allowed vaccination exemptions based upon medical contraindication or religious belief.
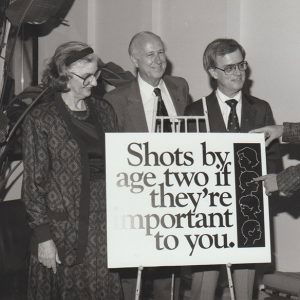
Despite passage of the 1967 law, immunization levels among Arkansas’s schoolchildren remained low. In 1973, Arkansas First Lady Betty Bumpers responded to the situation by launching her “Every Child by ’74” vaccination campaign. Bumpers later recalled that “we immunized several hundred thousand kids one Saturday [in 1973].” Other states modeled their own immunization programs on her successful campaign.
For some, however, the very success of vaccination shifted their focus away from the risks of disease to the perceived risks of the vaccines themselves. In the 1980s and the 1990s, concerns about vaccine safety fueled a resurgent anti-vaccination movement. In 1998, British physician Andrew Wakefield’s now-retracted paper, published in the Lancet journal, fraudulently linked the MMR vaccine to the development of autism and bowel disease in children. Other allegations surfaced that the preservative thimerosal, which has been removed from most vaccines, caused autism. Although subsequent research showed no evidence of harm caused by either the MMR vaccine or thimerosal, many opponents of vaccination remained unconvinced.
In the 1990s and the early 2000s, some states, including Arkansas, adopted philosophical/personal-belief vaccination exemptions. In Boone v. Boozman (2002) and McCarthy v. Boozman (2002), the federal courts upheld Arkansas’s school vaccination mandate but ruled that Arkansas’s method of providing religious exemptions unconstitutionally permitted government officials to decide which religions they would recognize and which they would not. In 2003, the Arkansas General Assembly passed legislation authorizing the state health department to grant philosophical/personal-belief vaccination exemptions.
By 2016, children and teenagers, in order to receive admission into Arkansas’s childcare facilities and schools, were required to certify legally that they had been vaccinated against diphtheria, pertussis, tetanus, measles, mumps, rubella, hepatitis A and B, Haemophilus influenzae type b (a cause of meningitis), pneumococcal and meningococcal diseases, and chicken pox. College students also had to certify that they had been immunized.
Individuals must annually apply to the Arkansas Department of Health for medical or nonmedical (religious or philosophical) school vaccination exemptions. All applicants are required to submit a notarized exemption request, and applicants for medical exemptions must submit a physician’s statement of medical contraindication. Other requirements include completing state health department–sponsored immunization education; completing a medical, religious, or philosophical exemption form; and signing an “informed consent” form. The consent form includes a statement of vaccine refusal and a statement of understanding that, during an outbreak of disease, an unvaccinated person may be removed from a facility until the outbreak is resolved. Employees of nursing homes may apply for a medical exemption from the influenza (“flu”) vaccine.
In 2015, among Arkansas’s children, only sixty-six percent of children nineteen months to thirty-five months old received vaccinations, compared with 71.6 percent nationally. During the school term of 2014–15, 6,058 unvaccinated or under-vaccinated children attended Arkansas schools. The number of philosophical exemptions granted to Arkansas’s schoolchildren rose from 403 in 2003 to 4,311 in 2015. The number of religious exemptions rose from 297 in 2003 to 1,583 in 2015. In 2003, sixty-four children received medical exemptions. In 2015, 164 children were medically exempted. By the 2018–2019 school year, more than 8,000 children received exemptions; only two percent of these were for medical reasons, while the remainder were for religious or philosophical reasons. The percentage of kindergarten students with non-medical vaccine exemptions reached an all-time high of 3.4 percent in Arkansas for the 2023–2024 school year but increased yet again the following school year to 3.6 percent.
The continuing challenge for Arkansas’s public health officials and medical professionals is to protect herd immunity by maintaining high vaccination levels in the population and simultaneously ensure fair exemptions. The state health department supplies vaccines to ninety-four local health departments and more than 500 non-health-department offices in Arkansas. Vaccinations for children and adults, excepting those required for international travelers, are available at Arkansas’s local health departments. Only certain physicians in Arkansas provide international travel vaccinations. Launched in 2013, Arkansas’s computerized immunization registry, known as WebIZ, serves as a confidential and centralized vaccination record database for use by medical professionals.
For additional information:
“Arkansas State Board of Health: Immunization Policies, 1960.” History of Public Health in Arkansas. Health Maintenance Records, Box 9, File 5. Historical Research Center. University of Arkansas for Medical Sciences Library, Little Rock, Arkansas.
Arkansas Department of Health. “Immunizations.” https://www.healthy.arkansas.gov/programs-services/topics/immunizations (accessed August 31, 2022).
Arkansas Department of Health. “Rules and Regulations Pertaining to Immunization Requirements, September 1, 2014.” https://www.healthy.arkansas.gov/images/uploads/pdf/ImmunizationRequirements.pdf (accessed August 31, 2022).
Cima, Michael J., Christina Joshua, Namvar Zohoori, Austin Porter III, Derek Slagle, Jennifer Dillaha. “Heistancy towards Routine Childhood Vaccinations before and after the COVID-19 Pandemic in Arkansas.” Vaccine 66 (November 14, 2025). https://doi.org/10.1016/j.vaccine.2025.127834 (accessed October 27, 2025).
Colgrove, James. State of Immunity: the Politics of Vaccination in Twentieth Century America. Berkeley: University of California Press, 2006.
College of Physicians of Philadelphia. “History of Anti-Vaccination Movements.” http://www.historyofvaccines.org/content/articles/history-anti-vaccination-movements (accessed August 31, 2022).
Duffy, John. “School Vaccination: The Precursor to School Medical Inspection.” Journal of the History of Medicine and Allied Sciences 33 (1978): 344–355.
Duval, Elias R. “Address on the Practice of Medicine.” Transactions of the Arkansas Medical Society 7 (1882): 50–54.
———. “Presidential Address.” Transactions of the Arkansas Medical Society 5 (1874):13–21.
Eblen, Anna L., and Martha Jane Eblen. Betty Bumpers: Champion of Immunization and Peace. Lanham, MD: Rowman & Littlefield Publishers, Inc., 2013.
Golden, Alex. “Unvaccinated Kids on the Rise across State, Health Data Show.” Arkansas Democrat-Gazette, April 15, 2019, pp. 1B–2B.
Miller, Elissa Lane. “From Private Duty to Public Health: A History of Arkansas Nursing, 1895–1954.” PhD diss., Memphis State University, 1989.
Mnookin, Seth. The Panic Virus: A True Story of Medicine, Science, and Fear. New York: Simon and Schuster, 2011.
Ngundue, Jerome Essono. “Disparities in Arkansas Mandated Immunization Coverage among Natural Home and Foster-Care Adolescents.” PhD diss., Walden University, 2016. Online at https://scholarworks.waldenu.edu/dissertations/2940/ (accessed August 31, 2022).
Offit, Paul A. Autism’s False Prophets: Bad Science, Risky Medicine, and the Search for a Cure. New York: Columbia University Press, 2008.
———. Vaccinated: One Man’s Quest to Defeat the World’s Deadliest Diseases. New York: HarperCollins Publishers, 2007.
Salmon, Daniel A., Jason W. Sapsin, Stephen Teret, Richard F. Jacobs, Joseph W. Thompson, Kevin Ryan, and Neal A. Halsey. “Public Health and the Politics of School Immunization Requirements.” American Journal of Public Health 5 (May 2005): 778–783.
Scholle, Sarah Hudson. The Pain in Prevention: A History of Public Health in Arkansas. Little Rock: Arkansas Department of Health, 1990.
Siebenmorgen, Lachan E. “Vaccination Hesitancy in the Arkansas Pregnant Population: An Exploratory Qualitative Study.” PhD diss., University of Arkansas for Medical Sciences, 2025.
Taggart, Sam. The Public’s Health: A Narrative History of Health and Disease in Arkansas. Little Rock: Arkansas Times Publications, 2013.
United Health Foundation. “America’s Health Rankings 2015: Arkansas.” http://www.americashealthrankings.org/AR (accessed August 31, 2022).
Wickline, Michael R. “Court Favors Mom in Girl’s Inoculations.” Arkansas Democrat-Gazette, June 25, 2021, pp. 1B, 3B.
Young, Frank B. “Report of an Epidemic of Smallpox in Washington County.” Flashback 7 (November 1957): 3–4.
Melanie K. Welch
Mayflower, Arkansas








Comments
No comments on this entry yet.