calsfoundation@cals.org
Rubella
Rubella or “German measles” is a contagious disease caused by a virus of the genus rubivirus, which is identified as a member of either the family matonviridae or togaviridae. Present only in humans, the rubella virus is unrelated to the measles virus. The disease acquired the name German measles because it was first described by German physicians in the mid-eighteenth century.
Typically a mild illness of childhood, rubella spreads from person to person through respiratory droplets, appearing following an incubation period of twelve to twenty-three days. Symptoms include a low-grade fever, enlarged lymph nodes, and a diffuse, fine, light-red rash. Recovery usually confers immunity.
Rubella is most dangerous during pregnancy. Prenatal maternal rubella infection, particularly if it occurs during the first trimester, can cause miscarriage, stillbirth, and premature birth, as well as Congenital Rubella Syndrome (CRS) in the infant. Children with CRS may exhibit one or more severe birth defects, including blindness, deafness, heart defects, and intellectual disability. During their first year of life, CRS patients’ viral shedding poses a risk to rubella-susceptible individuals.
As nineteenth-century physicians struggled to distinguish rubella from measles and other rash-causing illnesses, they used many additional names for the disease, including rotheln and rothelu. With his 1815 publication, “Some Account of a Rash Liable to be Mistaken for Scarlatina [scarlet fever],” British physician W. George Maton began the process of medically differentiating rubella from other diseases.
First proposed by British surgeon Henry Veale in 1866, the name rubella was derived from the Latin word rubellus, which meant “somewhat red.” During the London International Congresses of Medicine held in 1881, physicians failed to differentiate rubella formally. In 1898, Dr. George F. Hynes of Fort Smith (Sebastian County) noted rubella’s “difficulty of diagnosis” and observed that its “only proper synonyms [were] rothelu [and] German measles.”
As American troops prepared to enter World War I in 1917, they crowded into training camps and easily spread infectious diseases. Although a comparatively mild illness, rubella sidelined troops and spread into the community. In October 1917, rubella and measles erupted among the men stationed at Camp Pike (now Camp Joseph T. Robinson) in North Little Rock (Pulaski County). From his base in Lonoke (Lonoke County), Dr. Jacob C. Geiger, an epidemiologist with the United States Public Health Service, reported that hospitalizations for rubella and measles reached 1,200 men in December 1917. To make matters worse, the outbreak quickly spread to North Little Rock and Little Rock (Pulaski County). In 1918, Geiger observed that the immediate need for “proper diagnosis and differentiation…was evidently at first disregarded.”
Beginning in the late 1930s, physicians slowly advanced their understanding of rubella. In 1941, following a rubella epidemic that occurred in 1940, Australian ophthalmologist Norman McAlister Gregg noticed an unusual increase in cases of congenital cataracts among the local children. In “Congenital Cataract Following German Measles in the Mother,” he explained that prenatal maternal rubella infection caused the children’s conditions. Despite the medical community’s initial skepticism, others soon confirmed Gregg’s work.
During the rubella pandemic of 1962–1965, an estimated 12.5 million cases of the disease occurred in the United States, resulting in 20,000 cases of CRS, 11,250 fetal deaths, 2,100 neonatal deaths, and many therapeutic abortions. Efforts to develop a rubella vaccine accelerated.
In 1962, Dr. Paul Parkman and others at the Walter Reed Army Medical Center became one of the two groups to isolate the rubella virus successfully. In 1964, Parkman joined Dr. Harry M. Meyer Jr. at the National Institutes of Health (NIH), where they produced a live-attenuated rubella vaccine. Educated at Hendrix College in Conway (Faulkner County), Meyer graduated from the Arkansas Medical School, now the University of Arkansas for Medical Sciences (UAMS), in 1953.
In 1965, Parkman and Meyer collaborated with Dr. Theodore C. Panos, who was the Arkansas Medical School’s chair of pediatrics, to conduct their vaccine trials at the Arkansas Children’s Colony (ARCC) in Conway. Later renamed the Conway Human Development Center (CHDC), the ARCC was created as a residential educational institution for children with intellectual disabilities. Parkman, Meyer, and Panos obtained the consent of the trial participants’ parents. Although it would now be considered highly unethical, medical researchers formerly preferred to work with residents of institutions because they lived in easily monitored, isolated environments. Legal reforms of the late 1970s established informed consent as standard legal doctrine in the United States.
Parkman and Meyer’s vaccine produced immunity without communicability. In 1966, the ARCC’s medical director called the trial results “most satisfactory.”
American vaccinologists Dr. Stanley A. Plotkin of the University of Pennsylvania and Dr. Maurice R. Hilleman of Merck produced live-attenuated rubella vaccines, with Plotkin using human fetal cells and Hilleman using duck embryos. Originally licensed for use in 1969, Hilleman’s modification of Parkman and Meyer’s vaccine was replaced by Plotkin’s more effective vaccine in 1979. In 1971, the MMR (Measles, Mumps, and Rubella) vaccine became available.
Early vaccination efforts targeted one- to thirteen-year-olds because it was then unknown if the vaccine was safe to use during pregnancy. The rubella vaccine has proven to be very safe—little evidence has emerged to suggest that it harms the fetus. As a cautionary measure, however, the rubella vaccine is still not recommended for use during pregnancy.
In 1976, the United States recorded 12,491 rubella cases and twenty-three cases of CRS, which was down from 57,686 cases of rubella and sixty-eight CRS cases in 1970. By the 1990s, fewer than 300 cases of rubella occurred annually. Between 1991 and 1999, Arkansas reported no cases of rubella. Since 1995, foreign-born Hispanics have accounted for most of the rubella cases reported in the United States.
Conforming to the trend, Arkansas’s rubella outbreak of 1999 originated among Hispanic employees of a Fort Smith poultry processing plant. Between twelve and fourteen confirmed cases were reported. The Centers for Disease Control and Prevention (CDC) reported that six of the confirmed cases occurred in pregnant women, resulting in one documented stillbirth. The Arkansas Department of Health (ADH) cooperated with employers to implement workplace vaccination and reinstituted rubella immunity screening for women of reproductive age.
As per the CDC’s childhood vaccination schedule, the ADH recommends that children receive their first dose of the MMR vaccine at twelve to fifteen months and the second at four to six years. In the twenty-first century, rubella and CRS cases in the United States are usually associated with unvaccinated individuals and international travel.
For additional information:
Arkansas Department of Health. “Immunizations.” https://www.healthy.arkansas.gov/programs-services/topics/immunizations (accessed August 31, 2022).
Centers for Disease Control and Prevention. “Rubella Outbreak—Arkansas, 1999.” Morbidity and Mortality Weekly Report 50 (December 21, 2001): 1137–1139. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5050a3.htm (accessed August 31, 2022).
Centers for Disease Control and Prevention. “Elimination of Rubella and Congenital Rubella Syndrome—United States, 1969–2004.” Morbidity and Mortality Weekly Report 54 (March 25, 2005): 279–282.
Centers for Disease Control and Prevention. “Recommended Child and Adolescent Immunization Schedule, 2021.” https://www.cdc.gov/vaccines/schedules/hcp/imz/child-adolescent.html (accessed August 31, 2022).
Cooper, Louis Z. “The History and Medical Consequences of Rubella.” Reviews of Infectious Diseases 7 (March–April 1985): S2–S10.
“Correspondence: Dr. George F. Hynes.” Journal of the Arkansas Medical Society 23 (1898): 129–130.
Geiger, J. C. “Epidemic of German Measles in a City Adjacent to an Army Cantonment.” Journal of the American Medical Association 70 (June 15, 1918): 1818–1820.
“German Measles Vaccine Found: Tested in State.” Arkansas Gazette, April 28, 1966, pp. 1, 8A.
Hoeyer, Klaus, and Linda F. Hogle. “The Politics of Intent and Practice in Medical Research Ethics.” Annual Review of Anthropology 43 (2014): 347–362.
Horstmann, Dorothy M. “Rubella: The Challenge of Its Control.” Journal of Infectious Diseases 123 (June 1971): 640–654.
Meyer, Harry M., Jr., Paul D. Parkman, and Theodore C. Panos. “Attenuated Rubella Virus: Production of an Experimental Live-Virus Vaccine and Clinical Trial.” New England Journal of Medicine 275 (September 15, 1966): 575–580.
Offit, Paul A. Vaccinated: One Man’s Quest to Defeat the World’s Deadliest Diseases. New York: HarperCollins Publishers Inc., 2007.
Peters, Doug. “Three in Fort Smith Contract Rubella.” Arkansas Democrat-Gazette, September 16, 1999, p. 4B.
Peters, Doug. “Rubella Cases Likely to Increase.” Arkansas Democrat-Gazette, September 24, 1999, pp. 1B, 14B.
Reagan, Leslie J. Dangerous Pregnancies: Mothers, Disabilities, and Abortion in Modern America. Berkeley: University of California Press, 2009.
Reef, Susan E., Teryl K. Frey, Katherine Theall, Emily Abernathy, Cindy L. Burnett, Joseph Icenogle, Mary Mason McCauley, and Melinda Wharton. “The Changing Epidemiology of Rubella in the 1990s.” Journal of the American Medical Association 287 (January 23–30, 2002): 464–472.
Shores, Elizabeth F. “The Arkansas Children’s Colony at Conway: A Springboard for Federal Policy on Special Education.” Arkansas Historical Quarterly 57 (Winter 1998): 408–434.
“Vaccine Co-Developer Dies at Age 72.” Longview Daily News (Longview, Washington), August 26, 2001, p.10.
Melanie K. Welch
Mayflower, Arkansas
 Health and Medicine
Health and Medicine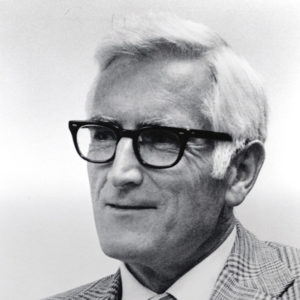 Harry M. Meyer
Harry M. Meyer  Harry M. Meyer
Harry M. Meyer 



Comments
No comments on this entry yet.